I have been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my competency i reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
CASE DISCUSSION:
A 76years old female housewife by occupation brought with complaints of
- chest pain since yesterday
- SOB since morning
HOPI:
Patient was apparently asymptomatic 2yrs and was diagnosed with hypertension (is on medication not known). 2yrs back was admitted at a private hospital for liver problem- cholelithiasis -done cholecystectomy.
Presently- complained of chest pain since yesterday associated with 2 episodes of Vomiting,Sweating and 2 episodes of loose motions.
Was taken to RMP and was given 1 injection and tablet and brought back to home.
Since today morning she complained of discomfort and was brought to casualty .
PAST HISTORY:
Not a k/c/o - DM,TB,ASTHMA,EPILEPSY
PERSONAL HISTORY:
She is Married
She consumes
- Mixed diet
- sleep is adequate
- Appetite normal
- bowel and bladder movements are regular
MENSTRUAL HISTORY: attained menopause 15 years back
FAMILY HISTORY:
No similar complaints in family
GENERAL EXAMINATION:
At time of admission
Pt is drowsy,extremities were cool and clamy
PR-75bpm
Bp-60/40mmhg
Spo2-57% ON RA
CVS-S1,S2 +, no added sounds
RS- b/l diffuse crepts on inspiration
P/A-Soft,NT Scar present at the right hypochondriac region (kochers incision for cholecystectomy)
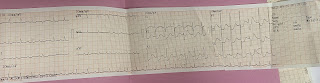
CLINICAL IMAGES:
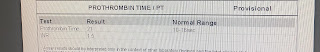
INVESTIGATIONS:
2D ECHO: https://youtu.be/D3m0t9MIGxU
ABG:Day1 at 4:40pm
Serum lactate: 31
DIAGNOSES: CARDIOGENIC SHOCK SECONDARY TO NSTEMI WITH CARDIOGENIC PULMONARY EDEMA.
TREATMENT:
PT WAS INTUBATED IN VIEW OF HYPOXIA AND CONNECTED TO MECHANICAL VENTILATOR
In view of cardiogenic shock pt was started on inotropic support
Post intubation vitals:
Bp:90/60MMHG
Pr:140BPM
Spo2:95%
Rr:crepts decreased
Post intubation investigations:


MEDICATION:
RT FEEDS 100ml milk 4th hrly, 50ml water 2nd hrly
Inj.PAN 40mg/IV/OD
Inj.Zofer 4mg/IV/SOS
Inj.NA 2 AMP IN 40ml NS @ 14ml/hr
Inj.doubutamine 1 amp in 45ml NS @ 15ml/he
Inj.Atracurium
Inj.Lasix 40mg iv/b
Tab Ecosprin AV 75/10 OD
Inj.Clexane 60 mg sc bd
inj.KCL 1amp in 200ml NS over 4 hrs
Vitals are monitored
Day 2
S: Pt is on mechanical ventilation and sedation
O:
Pt ACMV VC MODE
GCS: E1VTM1
RR TOTAL:23
RR:14
Fio2:100
TV:400
PEEP:5
VITALS:
BP: 110/60mmhg
PR: 138bpm
RR: 21cpm
Temp: 100.4f
GRBS: 193mg/dl at 7:00am
SYSTEMIC EXAMINATION:
CVS: s1,s2 no added sounds
P/A: not tender,Soft
RS:BAE+
K/c/o - HTN since 2 yrs
A: CARDIOGENIC SHOCK SECONDARY TO NSTEMI WITH CARDIOGENIC PULMONARY EDEMA.
P:
RT FEEDS 100ml milk 4th hrly, 50ml water 2nd hrly
Inj.PAN 40mg/IV/OD
Inj.Zofer 4mg/IV/SOS
Inj.NA 2 AMP IN 40ml NS @ 14ml/hr
Inj.doubutamine 1 amp in 45ml NS @ 15ml/he
Inj.Atracurium
Inj.Lasix 40mg iv/b
Tab Ecosprin AV 75/10 OD
Inj.Clexane 60 mg sc bd
inj.KCL 1amp in 200ml NS over 4 hrs
Vitals are monitored
ABG:Day 2 at 1:30am
ABG:Day 2 at 1:20am
ABG:Day 2at 10:50pm
Day 3
S: Pt is on mechanical ventilation and sedation
O:
Pt ACMV VC MODE
GCS: E1VTM1
RR TOTAL:18
RR:18
Fio2:100
TV:420
PEEP:5
VITALS:
BP: 100/60mmhg
PR: 149bpm
RR: 17cpm
Temp: 98.4f
GRBS: 197mg/dl at 7:00am
SYSTEMIC EXAMINATION:
CVS: s1,s2 no added sounds
P/A: not tender,Soft
RS:BAE+
K/c/o - HTN since 2 yrs
A: CARDIOGENIC SHOCK SECONDARY TO NSTEMI WITH CARDIOGENIC PULMONARY EDEMA.
P:
RT FEEDS 100ml milk 4th hrly, 50ml water 2nd hrly
Inj.PAN 40mg/IV/OD
Inj.Zofer 4mg/IV/SOS
Inj.NA 2 AMP IN 40ml NS @ 14ml/hr
Inj.doubutamine 1 amp in 45ml NS @ 15ml/he
Inj.Atracurium
Inj.Lasix 40mg iv/b
Tab Ecosprin AV 75/10 OD
Inj.Clexane 60 mg sc bd
inj.KCL 1amp in 200ml NS over 4 hrs
Neb:budecort and mucomist
Vitals are monitored
Day 4
S: Pt is on mechanical ventilation and sedation
O:
Pt SIMV VC MODE
GCS: E1VTM4
RR TOTAL:18
RR:18
Fio2:100
SPO2 - 94
TV:420
PEEP:6
VITALS:
BP: 80/60mmhg
PR: 116bpm
RR: 22cpm
Temp: 98.4f
GRBS: 187mg/dl at 7:00am
SYSTEMIC EXAMINATION:
CVS: s1,s2 no added sounds
P/A: not tender,Soft
RS: diffuse crepts + in all areas
K/c/o - HTN since 2 yrs
A: CARDIOGENIC SHOCK SECONDARY TO NSTEMI WITH CARDIOGENIC PULMONARY EDEMA.
P:
Starting NORAD
Monitoring vitals and GCS
ABG:Day4 at 6:20am
ABG:Day 4 at 1:20pm
2D ECHO REVIEW:
Day 5
S: Pt is on mechanical ventilation and sedation FEVER SPIKES SINCE YESTERDAY AFTERNOON
O: Pt SIMV VC MODE
GCS: E1VTM4
RR TOTAL:20
RR:20
Fio2:70
SPO2 - 100
TV:440
PEEP:6
VITALS:
BP: 100/60mmhg
PR: 110bpm
RR: 22cpm
Temp: 102.6f
GRBS: 161mg/dl at 7:00am
SYSTEMIC EXAMINATION:
CVS: s1,s2 no added sounds
P/A: not tender,Soft
RS: diffuse crepts + in all areas K/c/o - HTN since 2 yrs
A: CARDIOGENIC SHOCK SECONDARY TO NSTEMI WITH CARDIOGENIC PULMONARY EDEMA.
P:
Monitoring vitals and GCS
titrating sedation and monitoring the response


Day 6:
Day 7:
Day 8
S: Pt is on day 8 of mechanical ventilation
FEVER SPIKES Present
Icterus +
O: Pt CPAP VC MODE
GCS: E1VTM4
RR TOTAL:30
RR:14
Fio2:30
SPO2 - 91
PEEP:6
VITALS:
BP: 110/90mmhg
PR: 132bpm
RR: 34cpm
Temp: 103.3f
GRBS: 225mg/dl at 6:00am
SYSTEMIC EXAMINATION:
CVS: s1,s2 no added sounds
P/A: not tender,Soft
RS: diffuse crepts + in all areas K/c/o - HTN since 2 yrs
A: CARDIOGENIC SHOCK SECONDARY TO NSTEMI WITH CARDIOGENIC PULMONARY EDEMA.
P:
Plan for CECT in view of R hemiparesis
Plan for tracheostomy in view of prolonged ventilation
Day 9
Day 10
Day 11
S: Pt is on day 11 of mechanical ventilation
FEVER SPIKES Present
Icterus +
O: Pt on T-piece CPAP VC MODE
GCS: E1VTM4
Fio2:41
SPO2 - 100
PEEP:8
VITALS:
BP: 90/60mmhg
PR: 110bpm
RR: 34cpm
Temp: 102.3f
SYSTEMIC EXAMINATION:
CVS: s1,s2 no added sounds
P/A: not tender,Soft
RS: diffuse crepts + in all areas K/c/o - HTN since 2 yrs
A: CARDIOGENIC SHOCK SECONDARY TO NSTEMI WITH CARDIOGENIC PULMONARY EDEMA.
P:
Plan to extubate